Ketamin Therapy - The Secret to Beating Depression - The Medical Revolution you Should Know About
Table of Contents
In recent years, ketamine has emerged as a groundbreaking treatment for depression, offering hope to millions of people worldwide. Unlike traditional antidepressants, ketamine works rapidly and has shown promising results even in cases where other treatments have failed. This blog post explores the rise of ketamine therapy, its benefits, and real-life stories of its impact on patients suffering from depression.
The Rise of Ketamine Therapy
How Ketamine Became a Game-Changer in Mental Health
Ketamine, initially developed in the 1960s as an anesthetic, has recently emerged as a revolutionary treatment for depression. Unlike traditional antidepressants, which can take weeks to show effects, ketamine often provides relief within hours. Studies have shown that up to 70% of patients with treatment-resistant depression experience significant improvement after ketamine therapy. This rapid response has made ketamine a beacon of hope for millions struggling with severe depression and suicidal thoughts.
The FDA approved ketamine for use in depression treatment in 2019, further validating its potential. Clinics offering ketamine therapy have proliferated, with over 100 clinics opening in the U.S. alone in the past five years. This surge reflects the growing acceptance and recognition of ketamine as a viable mental health treatment.
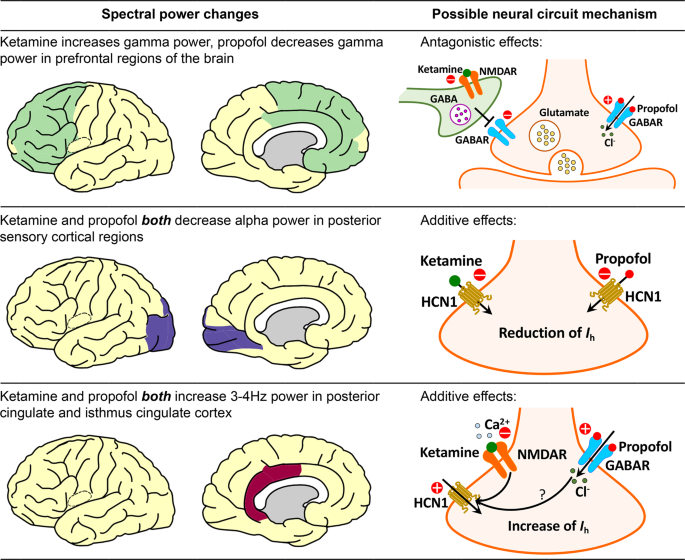
Moreover, ketamine’s unique mechanism of action, targeting NMDA receptors in the brain, sets it apart from other treatments. This distinct approach not only alleviates symptoms more quickly but also helps in repairing damaged neural connections, contributing to long-term mental health improvements. The rise of ketamine therapy marks a significant milestone in the ongoing battle against depression, offering a new pathway to recovery for those in need.
How Ketamine Therapy Works
Understanding the Science Behind Ketamine Therapy
Ketamine treats depression by affecting specific areas and mechanisms in the brain. It primarily works by blocking NMDA receptors, which are involved in the regulation of glutamate, a key neurotransmitter. This action increases gamma power in the prefrontal cortex, helping to enhance mood and cognitive function. Additionally, ketamine influences HCN1 channels, which play a role in neuronal excitability, leading to rapid antidepressant effects. By modulating these neural circuits and increasing the formation of new neural connections, ketamine can quickly alleviate depressive symptoms, even in patients who have not responded to other treatments..
Clinical studies have shown that up to 70% of patients with treatment-resistant depression respond positively to ketamine therapy. The effects are often felt within hours, providing swift relief from severe depressive symptoms and suicidal ideation.
Different Methods of Administration
Ketamine therapy is typically administered through intravenous (IV) infusions, allowing for precise control over dosage and immediate effects. A standard treatment regimen usually involves six infusions over two to three weeks, followed by maintenance sessions as needed. Other methods of administration include intranasal sprays and oral tablets, though IV remains the most effective.
The rapid and profound effects of ketamine therapy have positioned it as a groundbreaking treatment for depression, offering hope and relief for those who have struggled with traditional antidepressants.
Benefits of Ketamine Therapy for Depression
- Rapid Relief from Symptoms
One of the most significant advantages of ketamine therapy is its ability to provide rapid relief. Traditional antidepressants can take weeks to become effective, but ketamine often reduces depressive symptoms within hours. Research indicates that approximately 70% of patients with treatment-resistant depression experience substantial improvement after just one infusion.
- Effective for Treatment-Resistant Depression
For individuals who have not found success with conventional treatments, ketamine offers a new hope. Studies have shown that ketamine can be effective in cases where other antidepressants have failed. This makes it a valuable option for the estimated 30% of depression patients classified as treatment-resistant.
- Long-Term Mental Health Benefits
Beyond immediate symptom relief, ketamine therapy has been found to contribute to long-term mental health improvements. By promoting the growth of new neural connections, ketamine helps in repairing the brain’s damaged circuits, which can lead to sustained mood stabilization and cognitive function. Regular maintenance sessions can help prolong these benefits and prevent relapse.
- Minimal Side Effects
While all treatments have potential side effects, those associated with ketamine are generally mild and temporary. Common side effects include dizziness and nausea, which typically subside within a few hours after treatment.
Ketamine therapy stands out not only for its rapid and effective relief but also for its long-term benefits and manageable side effects, making it a promising option for those battling severe depression.
Our Patient Recovery Stories



Frequently Answered Questions
What are the main factors that cause OCD to get worse?
Stress and anxiety, changes in routine, sleep deprivation, and hormonal changes are some of the primary factors that can exacerbate OCD symptoms.
How does stress impact OCD symptoms?
Stress increases cortisol levels, heightening anxiety and making it more challenging to manage obsessive thoughts and compulsive behaviors.
Can poor sleep worsen OCD symptoms?
Yes, sleep deprivation can significantly impact mental health, increasing anxiety and reducing the ability to manage OCD symptoms effectively.
What role do hormonal changes play in worsening OCD?
Hormonal fluctuations, particularly during puberty, pregnancy, and menopause, can affect mood and anxiety levels, leading to an increase in OCD symptoms.
How does substance abuse affect OCD?
Substance abuse, including alcohol and drugs, can worsen OCD symptoms by increasing anxiety and making it harder to manage compulsions.
Why does a change in routine make OCD worse?
People with OCD often rely on structured routines to manage their symptoms. Disruptions to these routines can cause significant anxiety and exacerbate OCD symptoms.
Can a poor diet contribute to worsening OCD?
Yes, a poor diet lacking essential vitamins and minerals can affect brain function and mood regulation, potentially worsening OCD symptoms.
How can environmental factors influence OCD symptoms?
Environmental factors such as pollution, noise, and certain chemicals can exacerbate OCD symptoms by increasing anxiety and stress levels. Creating a calm and supportive living environment can help mitigate these effects.

About Dr. Prakhar D. Jain
Dr. Prakhar D. Jain is an experienced psychiatrist specializing in child and neuropsychiatry. With an impressive background that includes an MBBS, M.D. in Psychiatry, and PDF in Emergency Mental Health (USA), Dr. Jain provides comprehensive mental health solutions through his practice at Sir JJ Hospital, Wadia Hospital, and Royal Clinic in Mumbai.
For more information or to schedule a consultation:
Initiatives by Dr. Prakhar Jain
- IKIGAI: Comprehensive treatment for neurodevelopmental disorders.
- Sobriety: Effective de-addiction services.
- The Psychiatrist Says: Telepsychiatry and teletherapy for accessible mental health care.
- Centre of Excellence for Psychiatry & Neurology: Comprehensive dementia and old age issue management.
- Intimacy Intervention: Solutions for intimate issues affecting sexual satisfaction and fertility.
- The Soul Spa: Complete mental and emotional health solutions through advanced methods like biofeedback and behavioral therapy.
Understanding and managing stress is not just about surviving; it’s about thriving. Take control of your mental health with the guidance of Dr. Prakhar D. Jain and make stress management a priority in your life.

Dr. Prakhar D. Jain
MBBS, M.D. (PSYCHIATRY), PDF, EMH (USA)
Child & Neuro Psychiatrist.
Dr. Prakhar Jain is a Psychiatrist in Mumbai, and has an experience of 7 years in this field. Dr. Prakhar Jain practices at Sir JJ Hospital, Wadia Hospital & Royal Clinic in Mumbai. He completed MBBS from Indira Gandhi Government Medical College, Nagpur and M.D. (Psychiatry) from Grant Medical College and Sir JJ Hospital, Mumbai.